Psychiatry Soap Note Template
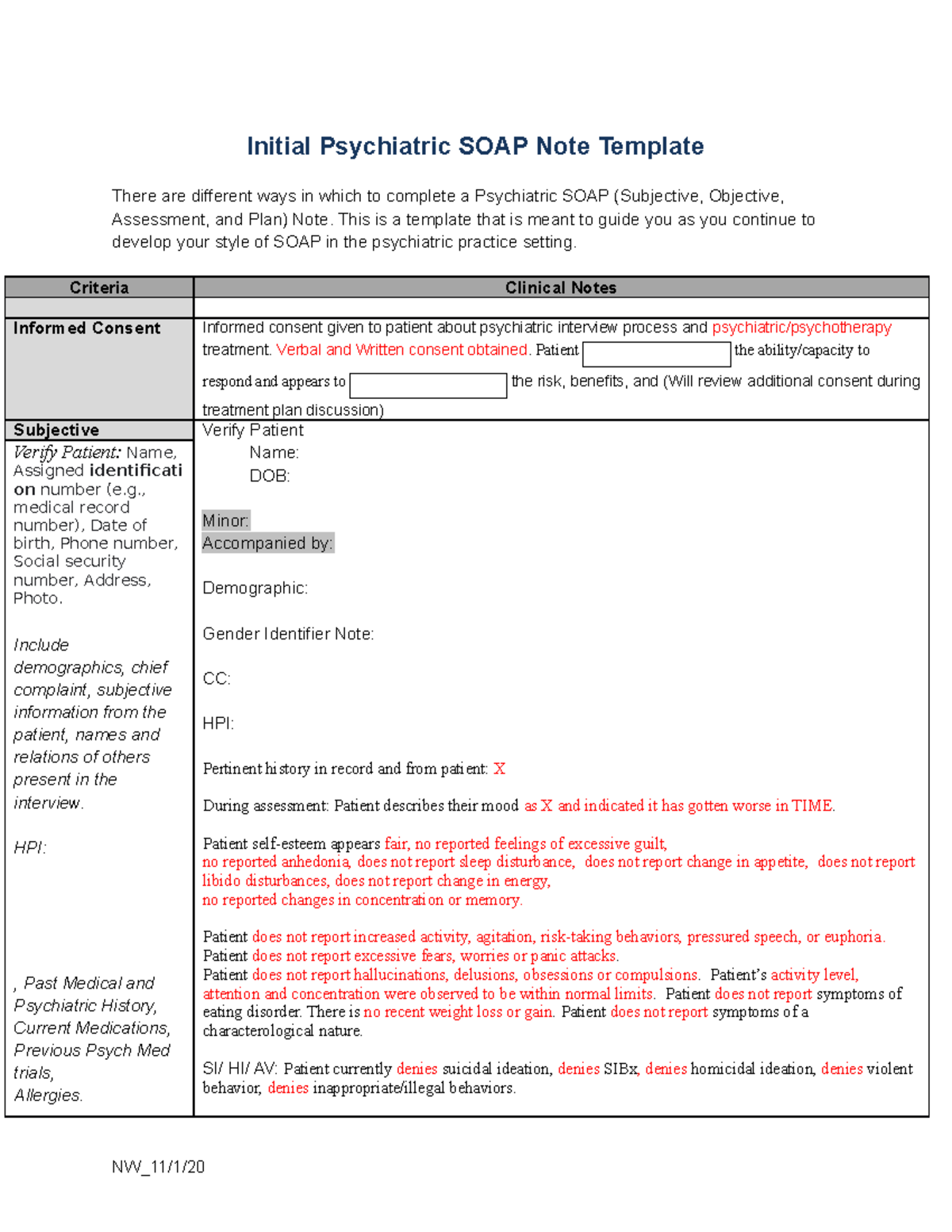
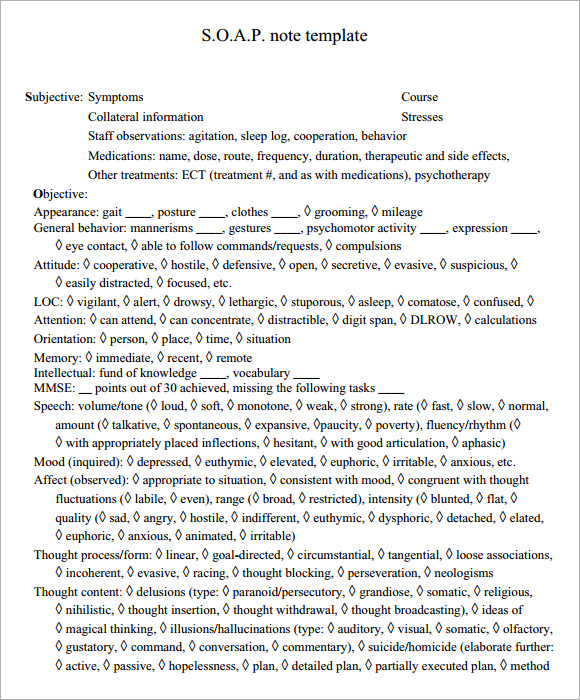
Psychiatry Soap Note Template - Depressive symptoms have improved but he still feels. Download our soap notes template pdf file right now. This is a template that is meant to guide you as you. The only words typed by the clinician are highlighted in yellow. She was first hospitalized in her twenties. Jan has been hospitalized on a number of occasions. Web there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Presented on time for scheduled counseling session engaged and cooperative avoidant or disengaged. Web initial psychiatric soap note template there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Not to be confused with the mini mental status exam. Web psychiatric initial evaluation template psychiatric progress note psychiatry soap note psychiatric discharge summary therapy initial assessment therapy progress note. Web past psychiatric history : Documentation is never the main draw of a helping profession, but progress notes are essential to great. Web the patient identifies the following symptoms: She was first hospitalized in her twenties. Soap notes are a way of recording. Web this sample so ap note was created using the icanotes behavioral health ehr. 5+ psychiatric soap note examples; Web there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Web initial psychiatric soap note template there are different ways in which to complete a psychiatric. Not to be confused with the mini mental status exam. Pertinent system irritability mood instability heightened anxiety attention problems troubled by hallucinations. Web the patient identifies the following symptoms: Documentation is never the main draw of a helping profession, but progress notes are essential to great. Web mental status examination. Web there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Web psychiatric initial evaluation template psychiatric progress note psychiatry soap note psychiatric discharge summary therapy initial assessment therapy progress note. Web psychiatric soap note template. Calculator, csv ready, mental status. Presented on time for scheduled counseling session engaged and cooperative avoidant or. Calculator, csv ready, mental status. Web 670 case study psychiatric soap note template with rx there are different ways to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Web past psychiatric history : Web top 10 mental status examination this is the full deal. Download our soap notes template pdf file right now. Presented on time for scheduled counseling session engaged and cooperative avoidant or disengaged. Soap notes are a way of recording. She was first hospitalized in her twenties. Depressive symptoms have improved but he still feels. Web 670 case study psychiatric soap note template with rx there are different ways to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Web the patient identifies the following symptoms: Web past psychiatric history : 5+ psychiatric soap note examples; Web initial psychiatric soap note template there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Soap notes are a way of recording. Web top 10 mental status examination this is the full deal. Soap notes are a way of recording. Pertinent system irritability mood instability heightened anxiety attention problems troubled by hallucinations. Not to be confused with the mini mental status exam. Web psychiatric initial evaluation template psychiatric progress note psychiatry soap note psychiatric discharge summary therapy initial assessment therapy progress note. Depressive symptoms have improved but he still feels. Calculator, csv ready, mental status. Documentation is never the main draw of a helping profession, but progress notes are essential to great. Web this sample so ap note was created using the icanotes behavioral health ehr. Jan has been hospitalized on a number of occasions. This is a template that is meant to guide you as you. Web 670 case study psychiatric soap note template with rx there are different ways to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Web there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Pertinent system irritability mood instability. Web 670 case study psychiatric soap note template with rx there are different ways to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Web this sample so ap note was created using the icanotes behavioral health ehr. Web past psychiatric history : Not to be confused with the mini mental status exam. Jan has been hospitalized on a number of occasions. The only words typed by the clinician are highlighted in yellow. Presented on time for scheduled counseling session engaged and cooperative avoidant or disengaged. Pertinent system irritability mood instability heightened anxiety attention problems troubled by hallucinations. This is a template that is meant to guide you as you. There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Mental status examination & other. Web soap notes pdf template for mental health providers. 5+ psychiatric soap note examples; Calculator, csv ready, mental status. Web there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Soap notes are a way of recording. Web the patient identifies the following symptoms: Depressive symptoms have improved but he still feels. Web psychiatric initial evaluation template psychiatric progress note psychiatry soap note psychiatric discharge summary therapy initial assessment therapy progress note. Web mental status examination. Web psychiatric initial evaluation template psychiatric progress note psychiatry soap note psychiatric discharge summary therapy initial assessment therapy progress note. Web past psychiatric history : Web there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Documentation is never the main draw of a helping profession, but progress notes are essential to great. 5+ psychiatric soap note examples; Download our soap notes template pdf file right now. Pertinent system irritability mood instability heightened anxiety attention problems troubled by hallucinations. Depressive symptoms have improved but he still feels. Calculator, csv ready, mental status. Web this sample so ap note was created using the icanotes behavioral health ehr. Jan has been hospitalized on a number of occasions. She was first hospitalized in her twenties. Web mental status examination. Web top 10 mental status examination this is the full deal. Presented on time for scheduled counseling session engaged and cooperative avoidant or disengaged. Web the patient identifies the following symptoms:NU646 Initial Psychiatric SOAP Note Template Initial Psychiatric SOAP
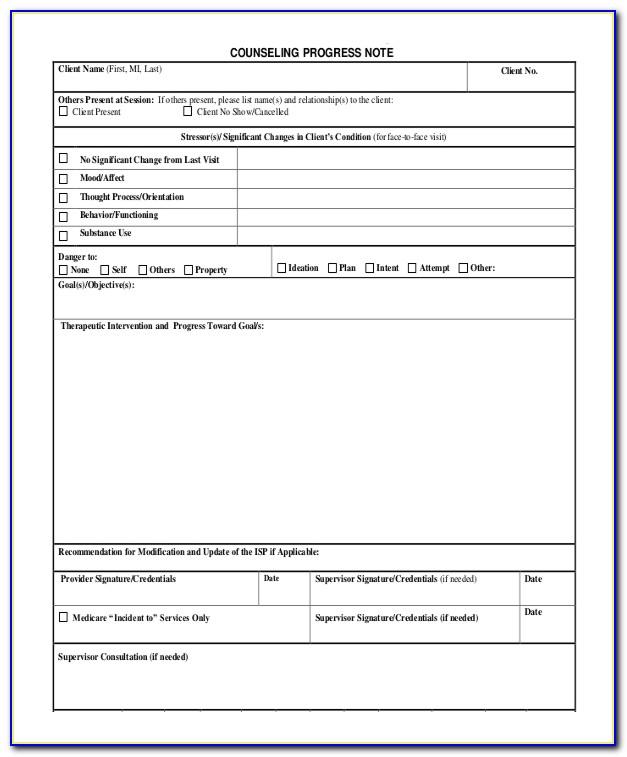
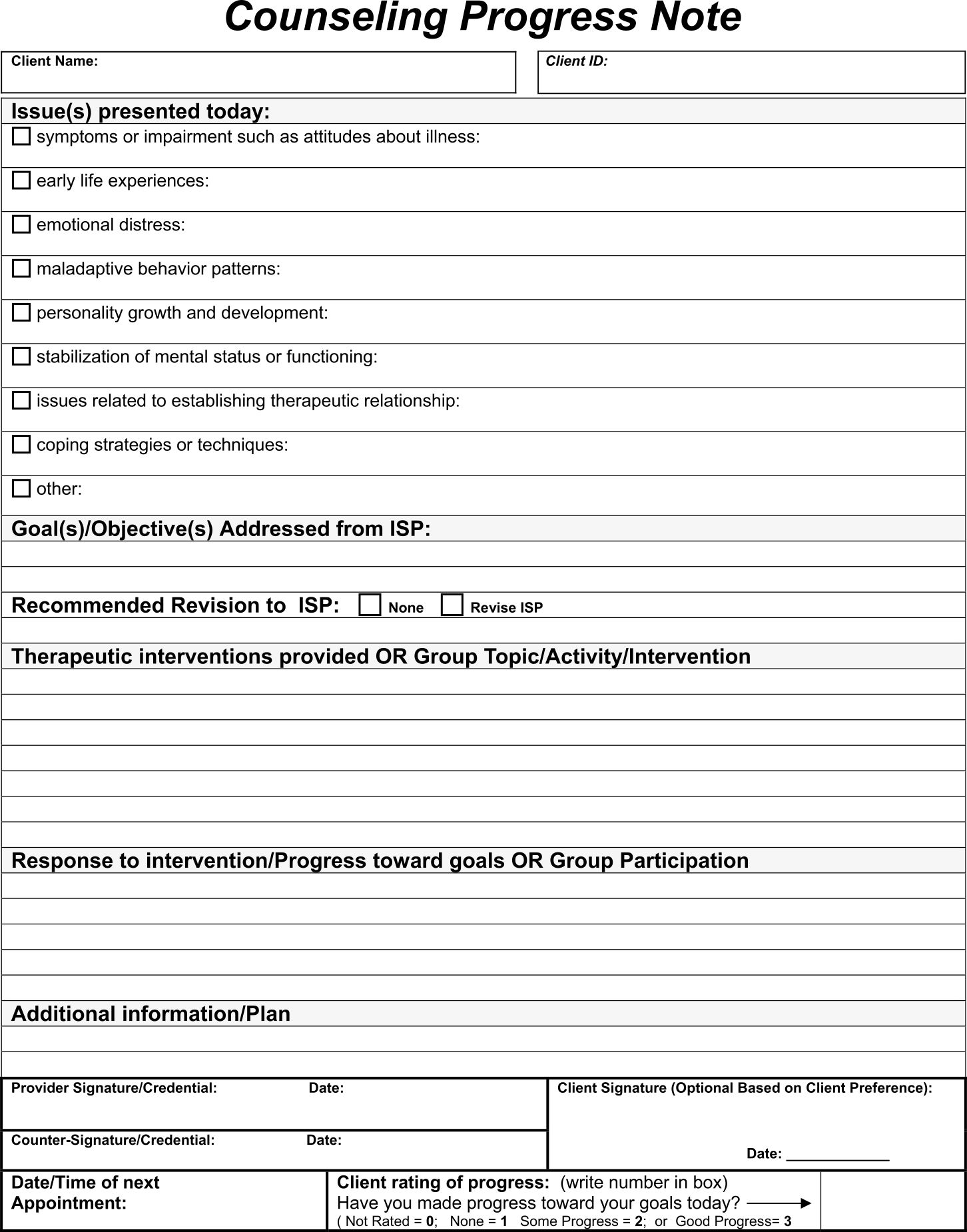
4+ Soap Notes Example Counseling in 2021 Therapy worksheets, Couples
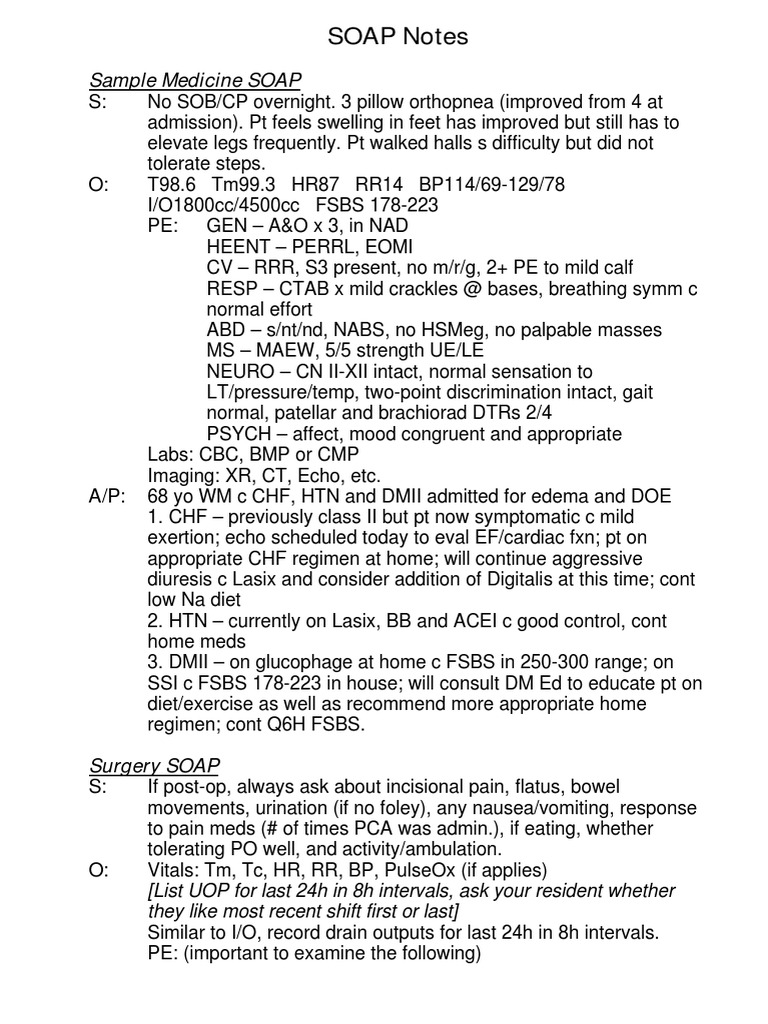
Psychiatric Soap Note Template
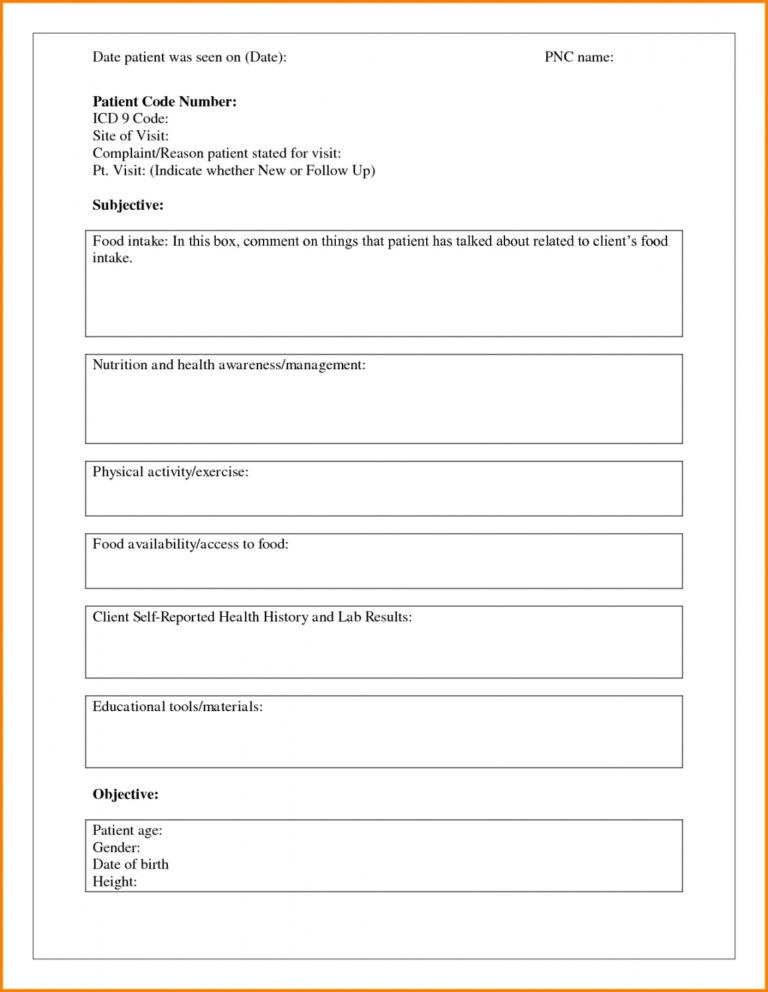
10+ Soap Note Template Free Download Word, Excel, PDF Format!!
29+ Psychiatric Soap Note Example Pics Nalo
Psychiatric soap Note Example Peterainsworth
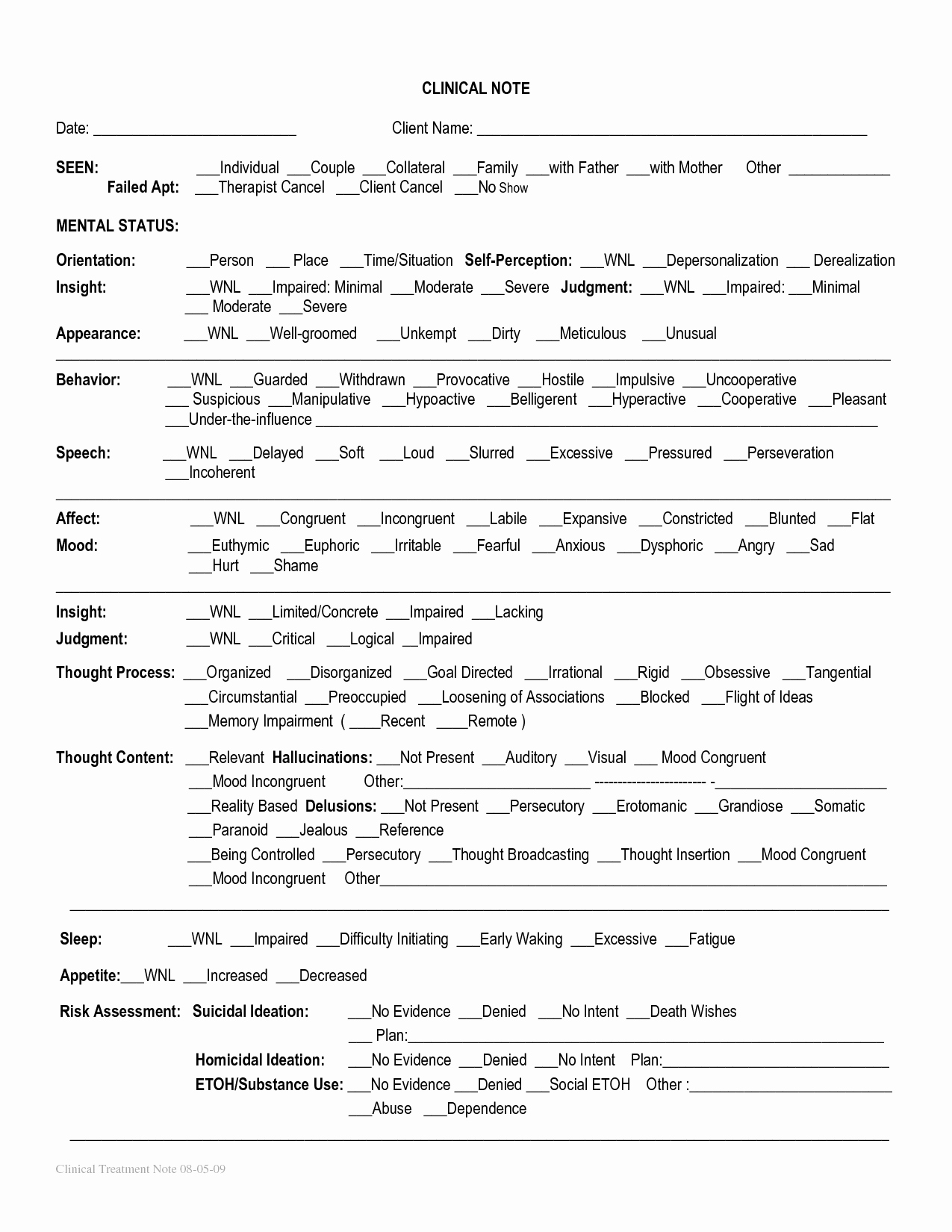
Pin on Therapy Tools
FREE 9+ Sample SOAP Note Templates in PDF MS Word
Printable Counseling Case Notes Template Printable Templates
Printable Soap Note Template Mental Health Heart Rate Zones Mental
Web 670 Case Study Psychiatric Soap Note Template With Rx There Are Different Ways To Complete A Psychiatric Soap (Subjective, Objective, Assessment, And Plan) Note.
This Is A Template That Is Meant To Guide You As You.
Web Initial Psychiatric Soap Note Template There Are Different Ways In Which To Complete A Psychiatric Soap (Subjective, Objective, Assessment, And Plan) Note.
There Are Different Ways In Which To Complete A Psychiatric Soap (Subjective, Objective, Assessment, And Plan) Note.
Related Post: